Excerpt from ” The Decision”
How I made my decision
When I began the process of determining which treatment option was best for me, I had not yet formulated the “who are you” concept. However, I used it intuitively as I had when working through the options over the years with patients of mine. My general health was good; all options were open to me. Cure, ease of treatment, and time out of work concerns were the most important factors to me and vied for the most prominent role in my decision. The risk of impotence and incontinence associated with surgical removal did not worry me as much as the complications and unknown future complications of radiation therapy. Having performed hundreds of prostatectomies over the years and knowing how my patients have done with surgery gave me some degree of confidence about my favorable chances of retaining continence and potency. I also had confidence in the treatments necessary for the correction of these issues if they were to occur. In my practice, the patients who did well with surgery usually did very well, without the unknowns and potential downside of radiation. The inability for those who chose radiation, and had problems, to do anything other than take medicines was a big factor in my decision. At the time of my diagnosis, I had some underlying early symptoms of an enlarged prostate, mild frequency and some decreased caliber of my urinary stream, and I knew that radiation would most probably worsen that. The fact that I was 52 played a role as well. I knew that my years at risk, figuring that I would most probably live into my 70s, would be over 20 years. This made me gravitate heavily toward what I felt was the most aggressive way to deal with the cancer. My path report was favorable in terms of Gleason’s score and volume, but my years at risk trumped this. The concern that cancer can return after radiation, not only because the cancer is outside the radiated field at the time of treatment, but because of the potential inability of radiation to kill the cancer, played a role here. Reoccurrence of prostate cancer after radiation, if it happens, usually happens five to eight years after treatment. The potential for inadequate placement with seeds heightened my concerns regarding my years at risk because those were probably longer than the average time to reoccurrence with radiation. In the end, my decision was driven by my belief that my best chance for cure was with surgery.

Summary of my decision – Now, you work through the “who are you?” factors the same way, as I did, for your situation.
- · Underlying health was good; all the options were open to me.
- · Cure vs. ease of treatment: cure was most important.
- · Time out of work a concern but trumped by desire for most aggressive treatment.
- · Unknown future effects of radiation concerned me more that the known potential complications of surgery. I felt that surgery was “cleaner” and that once I was over the surgery that would be it. (For me this has been the case.)
- · Having other treatment options if the cancer came back was important to me.
- · My underlying obstructive symptoms favored surgical removal, “killing two birds with one stone.”
- · My years at risk highly favored surgical removal.
- · Being a surgeon, I just plain felt more comfortable with surgery.
- · The influence of my friends and family was not a factor because I had my patients as models for how I might do with surgery. As a rule, they do quite well.
How you should make yours – Now it’s your turn
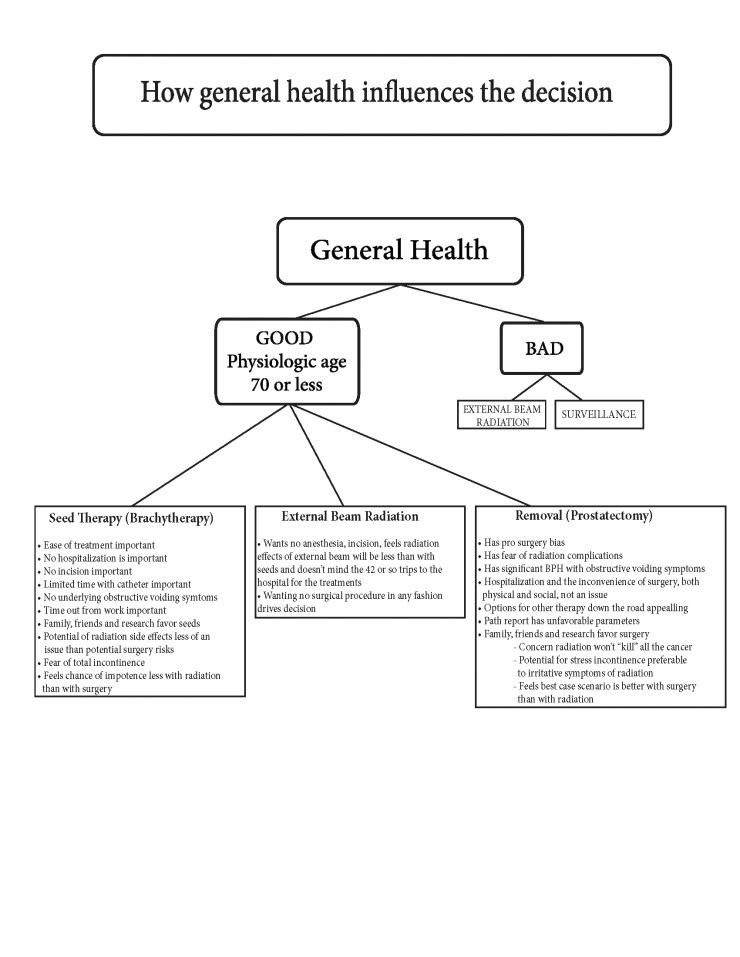
Armed with the information in this book, you too can come to a decision about your cancer’s treatment that you will become comfortable with. Begin with your general health and slowly work through which concerns trump others, and you will begin to narrow it down. The main point I’d like to make here is not to let your decision be one-dimensional (based on what a friend did, a commercial you saw, or a brochure you got in the mail). Ease of treatment, i.e. radiation, is a major concern for some; I explored that path as well. However, if you choose radiation because you feel there are fewer side effects, a better cure rate, or you are experiencing obstructive voiding symptoms, then you may be making an error. Have your radiation therapist thoroughly explain the negatives of radiation and be sure you are comfortable with his answers. If you have immediately gravitated to surgical removal, your health is marginal, and you are in your 70s, again you may be making the wrong decision. My advice is to explore all you know about your disease, your “who are you” factors, and discuss this with your health care providers to arrive at your decision.
My advice? Order “The Decision” and Patrick Walsh’s Book, speak to people who have gone through the process (remembering to compare apples to apples and oranges to oranges), and use as your internet resource the Prostate Cancer Page on the Johns Hopkins website. On that site find the Partin table and plug in your stats. This table will tell you the chances of having capsular extension of your prostate cancer. This is an important pre-decision distinction. If you think you want to have surgery because “I want to be done with it” but the Partin table tells you that you have a 25% chance of the PSA rising after surgery and that you’ll need additional radiation…will that make a difference in your decision making process? It would for me.
Now with all of the “Who are you?” factors addressed and you have done your homework-you are ready to make a decision. This process will not prevent the chances of a bad result, complications or side effects of your chosen treatment but it will limit them.




I started a community facebook page and have already had response. I called it High PSA Positive Biopsy. I began by discussing my own symptoms of progressive problems with maintaining erections during the last 12 months at the same time my PSA level was increasing from 5 to 8. The lesson learned is to advise other men to first of all have your PSA drawn every year after 50, but also do not ecnore symptoms of erection problems. That may be the only symptom that you need to see a urologist right away. Do not wait 4 of 5 years the way that I did. You are asking for the cancer to spread beyond the prostate if you do that.
I will live to regreat the fact that I waited too long before having a workup. You see I am a health care professional and knew what I was doing. There is no room for self distructive behavior in dealing with this disease. You have to do the right thing, regardless of how you feel at the time. Go see a urologist as soon as possible.
LikeLike
I kinda had my decision made for me. My prostate cancer was discovered first OUTSIDE the prostate. There were not many choices and having Crohn’s reduced them even more. My PSA has dropped to point three oh. I has all happened so fast. I wish I had some choices.
LikeLike
Interesting perspective as a surgeon. Thanks for the insight.
LikeLike
As I work my way through the treatment decision, I find myself gravitating to either Proton Radiation Treatment or HIFU – high frequency focused ultrasound but I am surprised that you make no mention of either of these options.
LikeLike
thanks…..addressed with today’s post….if you don’t want to have it removed then you are using some sort of energy to kill it. Iceberg Fineberg they’re all the same to me-pick your poison. hope it helps and good luck with your decision. ps….if you are young and healthy think aggressive, if older with other medical issues think surveillance or treatments aimed at the favorable pathology crowd. jm
LikeLike
Your blog is extraordinary. I wish I had come across it before I had to make my treatment decision. As I see it now my parameters and perspective weren’t what they should have been. At this point, I’m just praying that I can do the right things so that I can leave my grandchildren with some fond memories. Keep up the good work with this site. The human race and medicine need more folks like you !
LikeLike
I already made my decision but your information just reinforced that I’m doing what’s best for me. I hope you catch that fish! Live long , love life… Thank you!!
LikeLike
Thank you and good luck!💉
LikeLike
Thank you so much for the guide! My husband is 66 & in good health – except his PSA doubled last year-18 to 33! After a Gleason score 7=4=3 he had focal laser ablation. PSA dropped to 6 – in 3 months was up to 10. Second MRI biopsy was staged at Gleason 8. After a 2nd FLA PSA has dropped to 5.5; but we’re not taking anymore chances. Hopefully it hasn’t metastasized…surgery will at least provide info on the lymph nodes.
LikeLike
Dr, McHugh – I just found your site and wish I did earlier. I’ve already undergone SBRT of 8 weeks with virtually no side effects other than more frequent bathroom breaks which has subsided. Recently notice slide evidence of periodic blood in urine and after reading all the comments of folks having clotting problems and voiding problems and .blood loss – I’m scared to death of what the future holds. I completed SBRT 2 months ago. I was detected early with low risk prostate cancer. Are all these problems with clots, blood loss and voiding inevitable? A certainty for the future?
LikeLike
The number I have seen for the probability of side effects down the road, radiation cystitis, is about 12%. So you will have some degree of this but that it causes all the problems to which you refer is relatively low. It is, however, a problem when it does occur. There is a blog on the site called “But I had my radiation five years ago,” you might search then read that. JM
LikeLike